This Boston doctor team flew their young children to Texas, turned their living room into a research office and are picking up extra shifts to cover for their sick coworkers and console terminal COVID-19 patients. And now a month in, Brittany Bankhead-Kendall, MD, MS, and Brian Kendall, MD, both 2013 graduates from Ross University School of Medicine, still view their sacrifices and unwavering healthcare commitment as their medical calling.
“Most of the time we do a good job of being mom, dad, spouse, physician and human all at once,” Brittany said. “But we got to where we didn’t feel like we could do the best for our kids at this time and have really good patient care.” Last month, they made the agonizing decision to send their eight-year-old son and two-year-old daughter to Brittany’s parents’ home in Texas so they could maximize their focus on patient care.
“We dived deep into the wave that is life,” Brittany explained. “That’s what we do. We pour ourselves into work. We can fully focus on this surge of COVID-19 that’s happening in Boston and we’re able to be all present and work late or pick up extra shifts. We can volunteer for extra research and be available. We are making their absence mean something.”
Hear the couple speak about their situation on WHDH Channel 7 TV News in Boston and on Boston 25 TV News.
Dual Doctor Household
Brian is an emergency room physician practicing with the Steward Medical Group and Brittany is a surgical critical care fellow and administrative chief at the Massachusetts General Hospital and Harvard Medical School program, both working in Boston.
Finding a love connection during their undergrad studies at Texas A&M University, Brian headed to the Peace Core in Albania and Brittany moved to Miami for graduate school. When Brian returned and Brittany graduated, they tied the knot and journeyed together to the Caribbean where Ross Med leaders encouraged them to become each other’s support system. “We learned how to do that since day one of medical school and we value it now that we’re in the hardest time of our career.”
Brittany said the couple is where they are today because of the Ross Med platform. “The months we spent on the island were very unconventional. Not everyone has a volcano erupt on the island next to them before a test and not everyone has a hurricane while they are trying to study,” she laughed. “Everything we went through during our time on the island completely prepared us to do all the things we’ve done thereafter. We have grown to become resilient through those experiences and those are absolutely the building blocks and tools that we’ve been able to utilize.”
Different Hospital Viewpoints
While both are immersed in COVID-19 care, they are experiencing different outlooks from their respective hospital settings. Brian has witnessed a large drop in the volume of patients entering the emergency room, thanks to the multiple nationwide messages asking sick patients to home care first. But the downside is that patients with other ailments and experiencing symptoms related to heart attacks and strokes aren’t voluntarily coming in either. And then there are patients who are complaining of symptoms that are not typical of COVID-19 such as abdominal pain but end up being related. “It’s not just a breathing issue. We are going in and battling a disease we have no cure for.”
In the intensive care unit (ICU), Brittany said it’s beyond busy. “We are completely pushed to the max, stretched entirely thin,” she said adding that there isn’t enough staff to cover the number of patients. “We keep expanding. We don’t say no to anyone. We keep making floors into ICUs and using floor nursing for ICU nursing. We are managing a lot of sick patients at numbers that would have been unthinkable in the past. But now we have no other options.”
Fear of the Disease
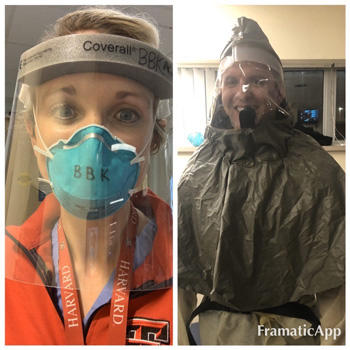
Both doctors know the reality that they too could become infected but take all the necessary precautions. Brittany said her fear has evolved from being initially scared about the physical components of the disease to now worrying about the emotional wellbeing of her patients and their families. Brian, who’s pleaded with legislators for coronavirus financial relief, added, “I’m more fearful of going to the grocery store than I am going to work because of how we were trained in medical school and in residency. You just learn to compartmentalize the dangerous aspects of it and make sure that you’re being as safe as you possibly can.”
And though Brittany said the situation has forced them to have those intense and difficult conversations with each other and family members about actions to take if either or both were to get sick, she said it’s even more grueling to witness her patients having end-of-life conversations on the phone or over video calls. Brian praised his wife for the extended emotional support she’s given patients. “She has sat by their bedside since the family can’t be there, playing their favorite songs or whispering the names of their family members until they pass. That alone is so heroic and for her, mentally and emotionally draining.”
Brittany credits her actions to her strong maternal nurturing side. “I consider it my ultimate privilege to be able to be there for those families and to do that because that’s what I would want for my loved ones.” And while she’s holding her patient’s hand inside the room, Brittany still must manage the 20-bed ICU by verbally directing residents on what to do next.
Reassuring Patients
“The hardest part now is calming the fears,” Brian said about informing patients who have tested positive for the coronavirus. “When you tell someone, you immediately see a wave of fear and just tears. You have long conversations and say we don’t know exactly what’s going to happen and tell them that the majority of people are going to recover. And that this is not by any means a death sentence, but everybody’s mind goes immediately there when they find out they have the virus.” And he has a message for others – “this disease is legitimate and no matter what your thoughts are on how it should have been handled or measures that are being taken, it has the ability to touch everybody’s lives whether that’s you getting sick personally or somebody whom you love. What we’re doing now is the only option we have to help control it.”
For now, Brittany and Brian hope their children are creating unforgettable memories with their grandparents. Brittany said she asked her son – who the couple lovingly calls their med school baby, “‘How is your heart? How are you feeling?’ And he'll tell us, ‘my heart’s in a million pieces because I miss you, but I know that you're with your patients and you're taking care of them and that's ok right now.’ So, he knows that we’re taking care of really sick people and that without us being there that they wouldn't have a chance to be with their families again.” Brian said, “I want him to remember how brave and courageous he had to be during this time, allowing us to be here.”
Dreams Coming True
Both dreamed of contributing to the medical field since a young age. Brittany remembers her kindergarten days of playing with heart-pump models and drawing in anatomy coloring books. Brian admired his grandfather, who practiced obstetrics and gynecology, and recalls dressing up as a doctor when he was a toddler.
And now that both have achieved their dream, they are also thankful of others fighting this fight with them. “It’s the most beautiful and harmonious thing about this from a community and global standpoint,” Brittany said. “Everyone has a part to play no matter how inconsequential or non-medical. Those roles really add up and allow healthcare workers to do their job on the frontlines. We’re eternally grateful.”
Appreciative and Thankful
We appreciate your commitment to the continued well-being of our Ross Med community and support during this unprecedented time. Please visit the Ross Med website for the latest updates regarding COVID-19.